CDC is working to increase sepsis awareness and improve treatment among the public, healthcare providers, and healthcare facilities. It kills more people than HIV/Aids, prostate cancer and breast cancer combined.
What is sepsis?
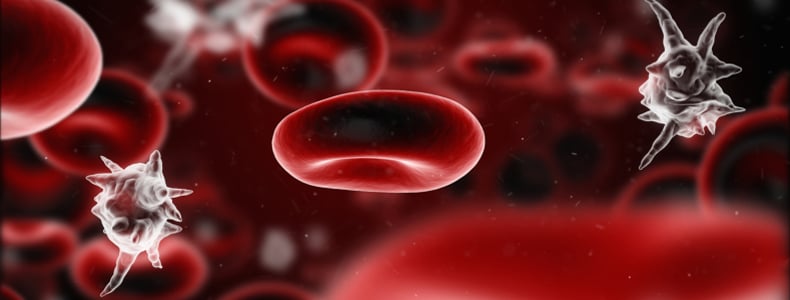
Sepsis is an illness that affects all parts of the body that can happen in response to an infection and can quickly become life-threatening.
In severe cases of sepsis, one or more organs fail. In the worst cases, sepsis causes the blood pressure to drop and the heart to weaken, leading to septic shock. Once this happens, multiple organs may quickly fail and the patient can die.
Sepsis is a serious illness that is very difficult to predict, diagnose, and treat. Patients who develop sepsis have an increased risk of complications and death and face higher healthcare costs and longer treatment.
What causes sepsis?
Sepsis is a response to an infection. When you get an infection, your immune system releases chemicals into your blood to fight the infection. The chemicals sometimes cause body-wide inflammation, which can lead to blood clots and leaky blood vessels. This impairs blood flow, which damages the body’s organs by depriving them of nutrients and oxygen.
Different types of infections can lead to sepsis, including infections of the skin, lungs, urinary tract, abdomen (such as appendicitis), or other part of the body. Healthcare-associated infections, including pneumonia, central line-associated bloodstream infections, catheter-associated urinary tract infections, and surgical site infections can sometimes lead to sepsis. MRSA infections of the skin and soft tissue can also lead to sepsis.
Who gets sepsis?
Anyone can get sepsis, but the risk is higher in:
- people with weakened immune systems
- infants and children
- elderly people
- people with chronic illnesses, such as diabetes, AIDS, cancer, and kidney or liver disease
- people suffering from a severe burn or physical trauma
How many people get sepsis?
CDC’s National Center for Health Statistics estimates that, based upon information collected for billing purposes, the number of times people were in the hospital with sepsis or septicemia (another word for sepsis) increased from 621,000 in the year 2000 to 1,141,000 in 2008.1
Between 28 and 50 percent of people who get sepsis die.2
The number of cases of sepsis each year has been going up in the United States. This could be because of the following reasons:
- the population is aging
- people have more chronic illnesses
- people are getting more invasive procedures, immunosuppressive drugs, chemotherapy, and organ transplants
- increasing antibiotic resistance
- increasing awareness and tracking of sepsis
Are there any long-term effects of sepsis?
Many people who survive severe sepsis recover completely and their lives return to normal. But some people, especially those who had pre-existing chronic diseases, may experience permanent organ damage. For example, in someone who already has kidney impairment, sepsis can lead to kidney failure that requires lifelong dialysis.
To learn more about Sepsis; visit the following resources: